Prostate-related urinary incontinence and retention are common problems in men, particularly with increasing age. Conditions affecting the prostate gland can interfere with normal urine flow and bladder control, leading to leakage, urgency, or difficulty emptying the bladder. In this page, we will highlight how the prostate affects bladder control, common prostate-related causes of urinary problems, diagnosis and treatment options.
How the prostate affects bladder control
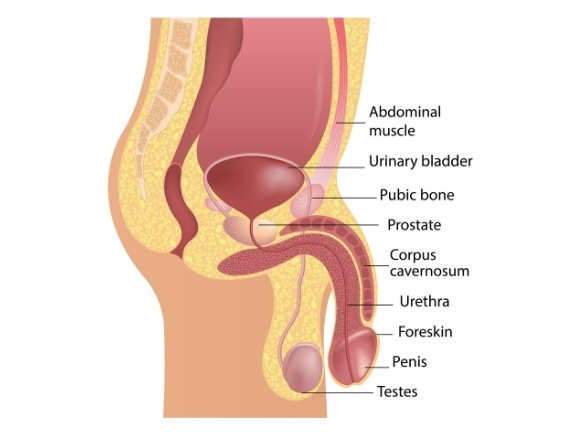
The prostate (a small gland in the pelvis) surrounds the urethra (the tube that allows urine to leave your bladder). If the prostate becomes enlarged or inflamed, this can restrict the flow of urine and lead to urinary incontinence.
Some prostate conditions, such as an enlarged prostate (Benign Prostatic Hyperplasia, or BPH) or prostatitis can lead to chronic urinary retention. This is where the bladder cannot fully empty. This blockage causes urine to build up, which over time puts pressure on the bladder walls, leading to stretching, thinning, and weakening of the muscle.
In the UK, about 1 in 3 men over 65 will experience urinary incontinence issues.1
Note to readers: According to research from AgeUK, the word “pee” is generally preferred over “urine”, so we’ve used it consistently throughout this page.
Common prostate-related causes of urinary problems
Enlarged prostate (also called Benign Prostatic Hyperplasia or BPH) is a condition affecting men, typically over the age of 50.
Not everyone with an enlarged prostate experiences symptoms, but common symptoms may include:
- Difficulty peeing or a weak stream of pee
- Feeling like you cannot empty your bladder
- Needing to pee more frequently
- Feeling a sudden urge to pee (urge incontinence)
Prostatitis is when the prostate becomes inflamed. It is thought that prostatitis is caused by an infection, such as a Urinary Tract Infection (UTI). Symptoms of prostatitis may include:
- Pain in your genitals or bottom
- Needing to pee more frequently
- Finding it painful to pee, experiencing a burning sensation
- Difficulty peeing
Prostate cancer and treatment for prostate conditions can cause urinary incontinence in men. Two of the most common treatments that can result in incontinence are:
Radiotherapy – Can irritate the bladder lining, causing a sudden urge to pee (urge incontinence). Other symptoms can include feeling a burning sensation when peeing and needing to pee more than usual.
Prostatectomy (surgery to remove some or all of the prostate gland) – This type of treatment can cause disruption to the urethral sphincter (two muscles used to control the exit of urine) and nerves.
Types of incontinence linked to prostate conditions
The type of urinary incontinence you have will depend on the condition you have. It is also possible to have more than one type.
Overflow incontinence
The most common prostate condition causing overflow incontinence in men is enlarged prostate. When the prostate is swollen, it blocks the urethra and prevents pee from being released fully from the bladder. If pee cannot be released from the bladder, it can cause a full feeling in the bladder, leaks, dribbling and difficulty peeing in general.
Urge incontinence
Urge incontinence is linked with prostatitis and enlarged prostate which both create a sudden and overwhelming need to pee. Both of these conditions can irritate the bladder and and cause dysfunction. For those with prostatitis, the inflammation of the prostate can interfere with nerves near the bladder, leading to sensitivity and contractions that cause the sudden urge to pee. An enlarged prostate can put pressure on the bladder, making it harder for the bladder to release pee. Over time, this pressure can make the bladder muscles weaker, resulting in urge incontinence.
Stress incontinence
Stress incontinence can occur as a result of treatment, particularly prostatectomy (prostate removal). During prostatectomy, tissue that supports the urinary sphincter and pelvic floor muscles can be disturbed or removed, causing weakness. After surgery, leaks can happen during activities that put pressure on the abdomen, such as coughing or sneezing.
Not all men experience incontinence after prostate removal, although it is a common, known side-effect of treatment.
Symptoms of prostate-related urinary incontinence
The symptoms you experience will depend on the condition you have, and the type of incontinence you have as a result. Some common symptoms of prostate-related urinary incontinence include:
Weak or interrupted stream
Difficulty peeing
Needing to pee frequently, especially at night (nocturia)
Sudden urges to pee
Leakage or dribbling
Feeling of incomplete bladder emptying

How prostate-related urinary problems are diagnosed
Here are some ways a healthcare professionals may diagnose prostate-related urinary issues. They may use a combination of different methods.
GP assessment
Review of a bladder diary (if applicable) and symptom-based questionnaires, such as International Prostate Symptom Score (IPSS).
Pee sample
Used to detect abnormalities, infection and identify conditions like prostate cancer.
Digital Rectal Examination (DRE)
An examination of the size, texture and shape of the prostate.
Prostate-Specific Antigen (PSA) Test
A blood test that calculates PSA (a protein made by the prostate). The levels of PSA can help diagnose and detect abnormalities.
Scans
Transrectal Ultrasound (TRUS), a test measuring the prostate, or bladder scans.
Cystoscopy
A procedure whereby a small tube with a camera inside is inserted through the urethra to allow examination of the bladder, prostate and urethra.
Treatment options for prostate-related incontinence
The treatment and management of your condition will vary on a variety of factors, such as severity of your incontinence, incontinence type and overall health. Treatment options can include:
Medications
Alpha-blockers can be used to treat incontinence due to their positive effect on the bladder and prostate muscles. These drugs relax the muscles, helping to release pee and relieve symptoms of urge and overflow incontinence. 5-alpha reductase inhibitors are used in cases of enlarged prostate and work by reducing the size of the prostate and restore normal bladder function. Once the prostate becomes smaller, it will no longer put pressure on the bladder and so pee can be released easily.
Surgical and procedural treatments
Transurethral Resection of the Prostate (TURP) may be performed to relieve symptoms of an enlarged prostate. The surgery will remove any excess tissue that blocks the urethra to help restore the flow of pee. A prostatectomy is another surgical option, this can be used to treat prostate cancer or enlarged prostate. During the surgery, the prostate gland, or part of it, are removed.
Continence management
Management of your prostate-related incontinence can be through pelvic floor exercise (also called kegel exercise). These movements help strengthen the pelvic floor muscles which over time can improve bladder control. Bladder training is also a commonly-used management option. Bladder training aims to regain control over the bladder by teaching it to hold pee in and reducing trips to the toilet. Techniques for bladder training could include monitoring fluids, delaying peeing and going to the toilet at scheduled times.
Manage incontinence with continence products
Urinary sheaths
The CliniSure Urinary Sheath has been designed with comfort, privacy and security in mind. In this video, SecuriCare Continence Nurse, Anna Moseley shows how to apply and remove a sheath, how they work and getting the best fit.
Can be worn for up to 24 hours
Better leak protection vs continence pads when fitted correctly
Discreet, no-noise packaging
View the video transcript +–
So first thing I have here is a measuring guide. I’ll show you on the model I have here. If we went for this one it would be slightly too big. If it’s too big, it’s gonna come away, it’s not gonna work for you. But if you go too small, it’s gonna be uncomfortable, it’s gonna be tight, might be a bit restrictive. So for this particular model I would go for 28.
You might notice as well when you get your sheath, a product like this. This is what we call a hair guard. This goes over the top of the penis like so and if you have any hair helps to keep the hair back. Another product I would use is a barrier wipe. A barrier wipe is good for keeping the area clean but also it makes the area quite tacky so when you’re putting the sheath on it helps to keep it nice and tight. So I’m gonna put a little bit of this barrier film on first.
When you get the sheath you have a little part like this which you can tear down and when you get the sheath out, again it looks a little bit like a condom. So it goes on the end of the penis like so, you grab the tip of the penis on the inside and it just rolls down really simply and there’s an adhesive inside there which just attaches itself to the penis and cause this is the right size helps to keep it secure.
Sheaths are incredibly tacky, so you’re gonna need a way of how to take this off. If you still have your hair guard on, to remove it you just give it a little tear and it comes off nice and easily. You don’t have to have this on the whole time you could actually take this off as soon as you put the sheath on or you can keep it on the whole time. It’s whatever you’re comfortable with.
To help to take the sheath off, I would use a medical adhesive remover. Without using this if you’re taking them off everyday it’s gonna get quite sore cause as I mentioned it’s incredibly tacky. A little bit of a spray of the adhesive remover like so and what that’s doing is it’s breaking down the glue. What I tend to do then lift a little bit of the sheath and just spray in between the skin and the sheath, helps to release the adhesive and it comes off nice and easily. Once it’s off you just put this into your normal household waste.

Intermittent self-catheters
We offer a choice of hydrophilic and gel intermittent self-catheters in a variety of lengths to suit your needs.
The Curan® Male Advantage Hydrophilic Catheter features:
A smooth coating for low friction and prolonged lubrication
BlueGrip to aid hygienic touch free insertion
Soft polished eyelets to prevent irritation

Living with prostate-related urinary incontinence
Living with prostate-related urinary incontinence is an adjustment and can impact daily life, routines and emotional wellbeing. After diagnosis, people may struggle with:
Social gatherings and travel – Managing your condition away from home and in new environments can feel daunting, especially when it comes to accessible toilets
Low confidence – Diagnosis can evoke feelings of embarrassment and anxiety, causing low self-esteem
Exercise and physical activities – People may avoid being active through fear of leaks
You don’t have to face these new challenges alone. Charities like Prostate Cancer UK and Bladder & Bowel UK offer support and advice to help you. Through their online communities, you can share your concerns and questions with other people with incontinence.

When to seek medical help
Speaking to a healthcare professional about incontinence can feel daunting and embarrassing, but it’s really important to identify the issue early on. Early diagnosis can help to improve your symptoms and prevent long-term complications.
If you are experiencing trouble peeing, leaks, blood in your pee or feeling like your incontinence symptoms are getting worse, speak to your GP. If you are concerned about prostate cancer or are showing symptoms, it is always best to seek advice from your GP or specialist Nurse when these concerns arise.
Many people with incontinence live a happy, healthy life. Incontinence can be managed with simple changes, including pelvic floor exercises, bladder training, or an incontinence product.
Key takeaways
Enlarged prostate, prostatitis, prostate cancer and treatment for prostate-related issues can all cause incontinence
In the UK, about 1 in 3 men over 65 experience urinary incontinence
Prostate conditions can cause urge, overflow and stress incontinence
Some symptoms of prostate-related incontinence include: leaks, difficulty peeing and sudden urge to pee
Diagnosis for prostate-related incontinence could be through a Digital Rectal Examination (DRE), Cystoscopy, tests or scans
Treatment for prostate-related incontinence could be medication, surgery or lifestyle changes like pelvic floor exercise
Speak to your GP if your symptoms are sudden, worsening or impacting daily life
References
- Prostate Cancer UK, Let’s Talk About Incontinence [Website] https://prostatecanceruk.org/get-involved/campaigning/incontinence (Accessed 22 January 2026)
Support and resources
Find lots of helpful tips for living with incontinence in our resource library.

How to self-catheterise
Learn how to self-catheterise safely and comfortably with this step-by step guide.

Common causes of urinary incontinence
Learn the common causes of urinary incontinence (UI) and how they affect both men and women.

Bladder Diary
Track daily activities, fluid intake and bathroom visits with our free downloadable bladdery diary.

Your guide to catheter bags
Learn the different types of catheter bags, sizes and configurations to support comfort, discretion, and independence in your daily life.


