This case study, written by Community Specialist Nurse Anna Moseley, explores the use of the CliniSure urinary sheath system in a patient with Parkinson’s disease and multiple comorbidities, highlighting how a tailored continence solution helped reduce fall risk, improve sleep, and restore quality of life for both patient and caregiver.
Improving Sleep and Safety With a Urinary Sheath
Community Nurse Specialist
Anna Moseley
This case study, written by Community Specialist Nurse Anna Moseley, explores the use of the CliniSure urinary sheath system in a patient with Parkinson’s disease and multiple comorbidities, highlighting how a tailored continence solution helped reduce fall risk, improve sleep, and restore quality of life for both patient and caregiver.

Nocturnal incontinence in Parkinson’s:
Risks, routines, and real-life impact
Bladder dysfunction is a common complication across a range of neurological conditions, including multiple sclerosis, Parkinson’s disease, stroke, and spinal cord injury.1 Neurogenic lower urinary tract dysfunction arises when neurological control of the bladder and urethral sphincters is impaired, resulting in symptoms such as urgency, frequency, nocturia, incomplete emptying, and urinary incontinence.1 These symptoms are particularly prevalent in Parkinson’s disease, affecting approximately 60% of patients as the disease progresses.2
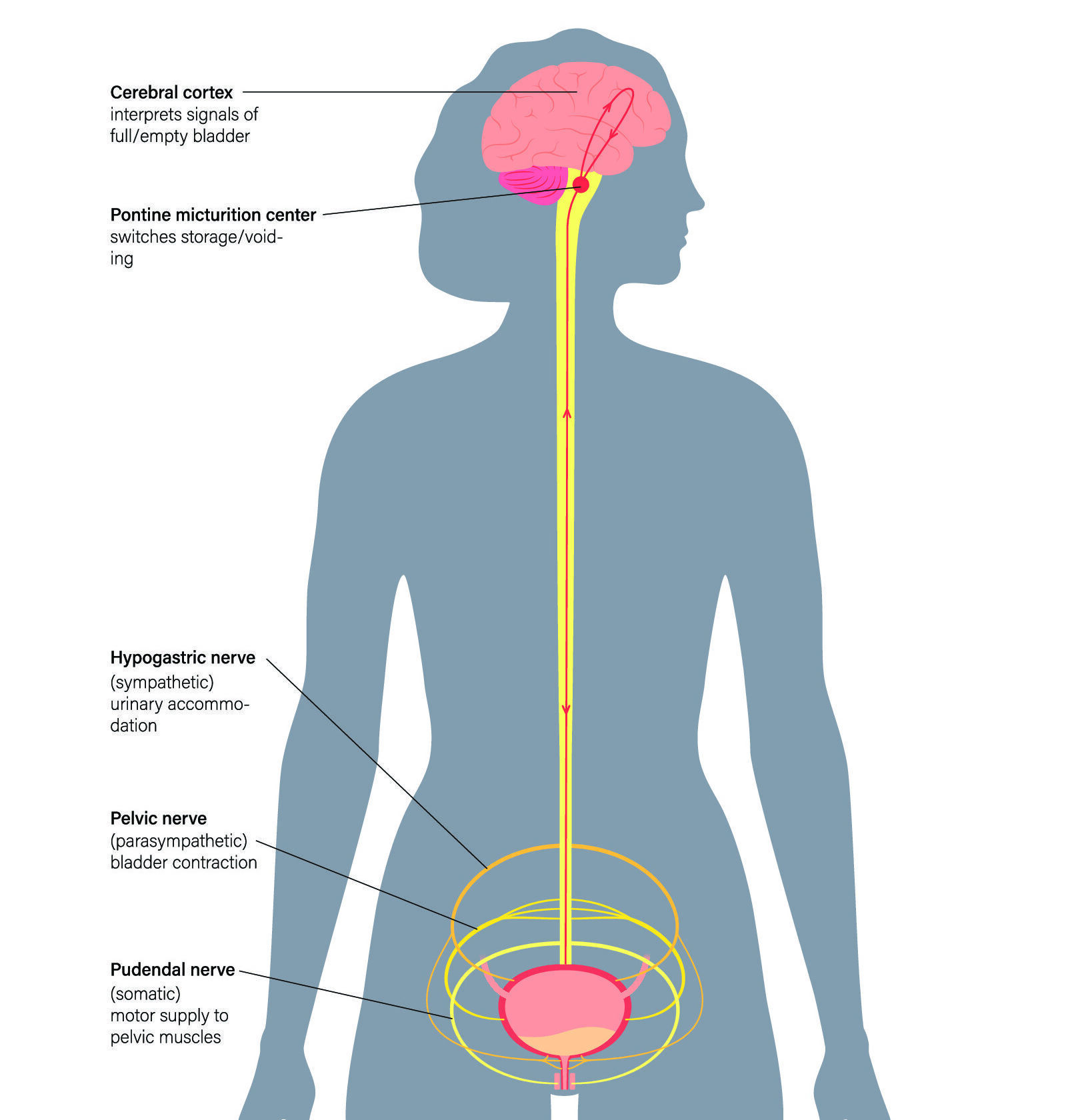
Neural control of the bladder involving the central nervous system and key peripheral pathways.
Disruption of these pathways, as seen in neurological disorders such as Parkinson’s disease, can contribute to bladder dysfunction.
Such urinary symptoms can have a significant negative impact on quality of life. Patients may struggle with embarrassment, disturbed sleep, or reduced independence, while caregivers, often spouses or family members, are faced with managing overnight episodes of incontinence, frequent laundry, sleep disruption, and the emotional strain of supporting a loved one through unpredictable episodes. When compounded by limited mobility, the risk of falls increases, particularly when patients attempt to reach the toilet unaided during the night.3
Management of bladder dysfunction in neurological conditions requires a personalised approach. Conservative strategies such as bladder training, pelvic floor exercises, and fluid timing are often first-line. Pharmacological options, including antimuscarinics or beta-3 agonists, may be considered, but can be poorly tolerated or contraindicated in older patients or those with polypharmacy. When symptoms persist, continence aids offer a practical and often essential layer of support.
Options range from absorbent products and urinals to more specialised solutions such as intermittent self-catheterisation (ISC), indwelling catheters, or external urinary sheaths.4 Among these, urinary sheaths can be an effective and discreet alternative for male patients, especially those with good urine output who cannot reliably access the toilet due to mobility issues. Clinical guidance recommends external continence devices as a non-invasive option in appropriate patients, particularly where carer support is available to assist with application and maintenance.4,5
This case study describes how the introduction of the CliniSure Sheath System, supported by specialised nurse intervention and carer involvement, helped to restore sleep, safety, and confidence in a patient with Parkinson’s disease and complex comorbidities.
Case overview:
Navigating urinary challenges in a patient with Parkinson’s disease
Mr Head is an 85-year-old male with a longstanding diagnosis of Parkinson’s disease. In general he maintains a good quality of life, living at home with his wife and occasionally enjoying short overnight holidays. However, following chemotherapy and radiotherapy for myeloma, Mr Head experienced a decline in mobility and he began waking nearly every hour during the night to urinate.
His need to stay well-hydrated, due to chronic kidney disease, further contributed to his night-time symptoms. With limited mobility, Mr Head faced increasing difficulty reaching the toilet safely overnight, raising concerns about his risk of falling.
The situation placed a growing strain on both Mr Head and his wife. She was frequently changing bed linen during the night and had moved to a separate bed due to disrupted sleep. The couple had stopped travelling overnight, and his wife expressed anxiety about his safety. In light of these challenges, Mr Head was referred by the Grimsby Continence team to a SecuriCare continence specialist nurse for further assessment.
Intervention:
Identifying a practical and dignified continence solution at home
During the initial home visit, the specialist nurse assessed Mr Head’s physical condition, continence needs, and daily care environment. His reduced mobility and frequent overnight urination, coupled with the risk of falls, were identified as key challenges. It was also evident that the impact extended beyond Mr Head, significantly affecting his wife’s sleep, wellbeing, and confidence in managing his care.
The nurse discussed a range of management options with Mr Head and his wife, including absorbent pads, a urinal, and the possibility of a catheter. Given the couple’s desire for a less invasive, more comfortable solution that would also support their goal of sleeping through the night safely, the nurse introduced a urinary sheath system.
With consent, a sheath assessment was carried out and a CliniSure urinary sheath was applied. Mr Head’s wife was actively involved throughout the demonstration and was shown how to apply and remove the sheath confidently. The nurse also provided a CliniSure night drainage bag and demonstrated how to securely affix and drain the system, ensuring both Mr Head and his wife felt comfortable managing the setup independently.
Continence products
Range of CliniSure urinary sheaths and night drainage bags.
We offer different sizes and styles to help ensure accommodation of varying patient needs, including overnight drainage solutions.
Outcomes:
Restoring routine, rest, and confidence through effective continence care
At a follow-up visit the following week, Mr Head and his wife expressed how transformative the introduction of the CliniSure sheath system had been. Since starting to use the product, they had not experienced any leakage, and for the first time in months, Mr Head was able to sleep through the night without needing to get up to urinate. His wife no longer had to change bed linen during the night and had returned to sharing a bed with her husband — a small but meaningful step in restoring their usual routine.
The emotional benefits were equally clear. Mr Head reported feeling more rested and secure, while his wife described feeling less anxious about night-time falls and more confident in supporting his care. Encouraged by the improvement, she had even booked a short overnight break for them both, something they had felt unable to consider before.
Eight months later, during a routine follow-up, the couple continued to report high levels of satisfaction with the product. The sheath system remained comfortable and reliable, and they noted the overall improvement in quality of life. For Mr Head, the solution helped preserve dignity and independence. For his wife, it provided reassurance and relief from the ongoing stress of managing night-time continence challenges — allowing them both to rest easier with a greater ease and comfort in daily life.
Key takeaways for healthcare professionals:
References
- Moussa M, Papatsoris A, Chakra MA, Fares Y, Dellis A. Lower urinary tract dysfunction in common neurological diseases. Turk J Urol. 2020;46(Supp. 1):S70-S78.
- Li FF, Cui YS, Yan R, Cao SS, Feng T. Prevalence of lower urinary tract symptoms, urinary incontinence and retention in Parkinson’s disease: A systematic review and meta-analysis. Front Aging Neurosci. 2022;14:977572.
- Diaconu Ş, Irincu L, Ungureanu L, Țînț D, Falup-Pecurariu C. Nocturia and Sleep in Parkinson’s Disease. J Pers Med. 2023;13(7):1053.
- National Institute for Health and Care Excellence (NICE). 2023. Urinary incontinence in neurological disease: assessment and management (CG148).
- National Institute for Health and Care Excellence (NICE). 2023. Lower urinary tract symptoms in men: management (CG97).





