This case study authored by Community Nurse Specialist Louise Harrison, reviews Curan Advantage with Tiemann Tip for a patient with benign prostatic hyperplasia addressing issues with insertion and improving confidence in managing to ISC independently.
Improving ISC Success for BPH Patients
The challenges of managing ISC in patients with BPH
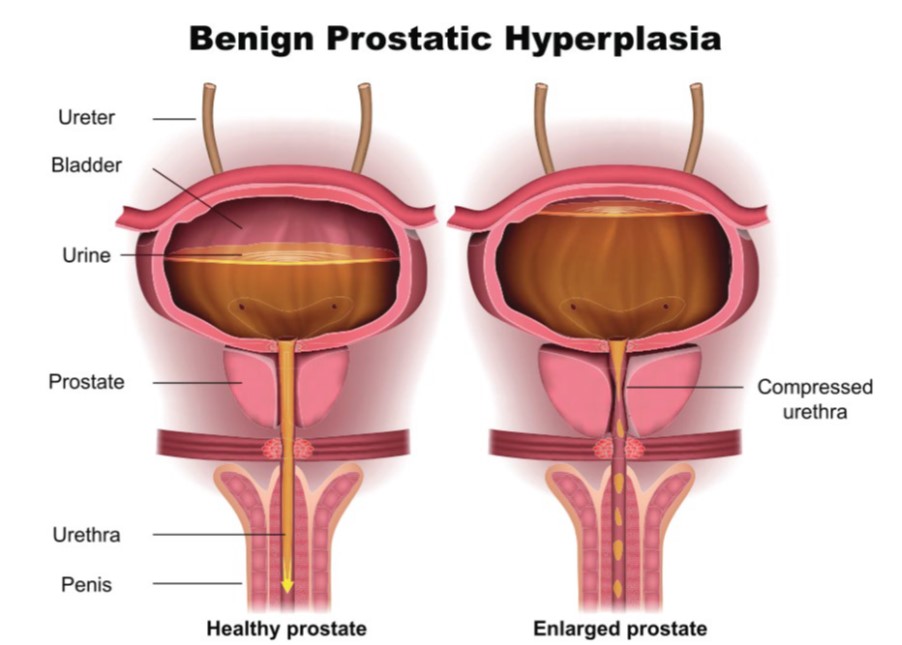
Benign prostatic hyperplasia (BPH) is a common condition affecting older men, with incidence increasing with age. By the age of 80, over 80% of men experience some degree of prostate enlargement.1 As the prostate enlarges, it can compress the urethra, leading to lower urinary tract symptoms such as weak urine flow, increased frequency, difficulty emptying the bladder and retention.2,3 These symptoms can significantly impact quality of life, often leading patients to seek medical intervention.4
Management of BPH varies depending on severity. Some patients are able to manage the symptoms with lifestyle modifications such as drinking less alcohol, caffeine and fizzy drinks, drinking less fluid in the evening, and exercising regularly.5 Medications, such as alpha-blockers and 5-alpha reductase inhibitors, can help relax the prostate or reduce its size and improve urine flow.5 Surgical options, including transurethral resection of the prostate (TURP) or minimally invasive procedures, may be required for severe obstructions.
Intermittent self-catheterisation (ISC) is a key non-surgical approach, particularly for patients experiencing chronic urinary retention who are not candidates for, or do not wish to undergo, surgery.6,7 It provides an effective way to manage urinary retention and avoid more invasive interventions such as indwelling catheters or surgery.
ISC can be particularly challenging in men with BPH due to urethral narrowing. Standard catheters may be difficult to pass, leading to discomfort, frustration and potential non-compliance.8 It can also be challenging for those with limited dexterity or mobility or those with other anatomical challenges that may hinder access.
Selecting the right catheter is key to long-term adherence and patient comfort. Research highlights that ease of use, nurse guidance and catheter design significantly influence whether a patient successfully continues ISC.9 The following case study illustrates how switching catheters helped a patient overcome these challenges and regain confidence in using ISC.
Case overview: Troubleshooting ISC in an 88-year-old patient
Charlie is an 88-year-old male patient who had been managing his urinary retention with ISC following a recent trial without a catheter (TWOC). He had received ISC training and had been advised to catheterise four times a day using a standard nelaton catheter.
Charlie was finding it difficult to insert the catheter successfully, often requiring multiple attempts before passing it into his bladder. He had no pain on catheterisation but was struggling to advance the catheter through the urethra. Compounding the issue, Charlie had limited manual dexterity and a large abdominal apron, which made locating the urethral opening more difficult.
Recognising these challenges, his community nurse team referred him to Community Nurse Specialist Louise for assessment and troubleshooting.
Intervention: Optimising catheter choice and technique
Louise visited Charlie at home to assess his technique and challenges:
- His overall technique was good, but he was repassing the same catheter up to four times if unsuccessful, increasing infection risk
- He was unaware that catheters are single-use only, and repassing could introduce bacteria
- The standard 14ch catheter was proving difficult to insert, likely due to the combination of BPH-related urethral narrowing, his limited dexterity and abdominal shape
To address these challenges, Louise introduced Charlie to the Curan Advantage Tiemann Tip catheter, which features a curved tip, allowing for easier insertion for someone with an enlarged prostate, and a blue guideline to assist with orientation and navigation. Additionally, she provided him with a smaller size (12ch) to see if this would ease insertion.

Outcome: Improved ISC success and greater patient confidence
With the Curan Advantage Tiemann Tip catheter, Charlie experienced immediate success:
- The blue guideline helped him correctly align the catheter, making insertion easier despite his limited visibility and dexterity
- The smaller 12ch size reduced resistance during insertion
- He quickly gained confidence, successfully catheterising on the first attempt
Charlie was supplied with a set of these catheters to ensure continuity of care during his upcoming holiday.
A follow-up after his trip confirmed that Charlie continued to self-catheterise without difficulty. He was able to fully empty his bladder, experienced no further complications, and felt more confident in his ability to manage ISC independently.
Key takeaways for healthcare professionals
This case underscores the importance of tailoring catheter choice to patient needs – particularly in those with BPH or anatomical challenges.
- Tiemann tip catheters are specifically designed to navigate the challenges of an enlarged prostate, improving ISC success
- A visual guide feature (i.e. the blue guideline) enhances alignment and control, particularly for patients with limited dexterity or visibility
- Correct catheter sizing is critical, downsizing from 14ch to 12ch in this case improved ease of insertion
- Patient education on best practices reduces infection risk and improves long-term adherence to ISC
- Provides patients with options that offer different features and benefits, taking their medical history into account when making recommendations
For patients struggling with ISC due to BPH or anatomical challenges, a Tiemann tip catheter, particularly one with a clear insertion guide like Curan Advantage Tiemann Tip, can make a significant difference.
This case study is based on real patient experience; identifying details have been anonymised to protect patient confidentiality. The information provided is education purposes only and should not replace clinical judgement or individualised patient care.
References
- GBD 2019 Benign Prostatic Hyperplasia Collaborators. The global, regional, and nation burden of benign prostatic hyperplasia in 204 countries and territories from 2000 to 2019. Lancet Healthy Longev. 2022 Nov;3(11):e754-e776.
- NHS. Benign prostate enlargement. June 2023. Available at: https://www.nhs.uk/conditions/prostate-enlargement/(Accessed: February 2025)
- NHS. Prostate problems. September 2021. Available at: https://www.nhs.uk/conditions/prostate-problems/ (Accessed: February 2025)
- The London Clinic. Benign prostate hyperplasia. Available at: https://www.thelondonclinic.co.uk/services/conditions/benign-prostate-hyperplasia-bph (Accessed: February 2025)
- NHS. Benign prostate enlargement – Treatment. June 2023. Available at: https://www.nhs.uk/conditions/prostate-enlargement/treatment/ (Accessed: February 2025)
- NHS. Intermittent self-catheterisation (ISC) for adults. July 2022. Available at: https://www.gloshospitals.nhs.uk/your-visit/patient-information-leaflets/intermittent-self-catheterisation-iscadults/ (Accessed: February 2025)
- Prostate Cancer UK. Enlarged prostate: A guide to diagnosis and treatment. May 2022. Available at: https://prostatecanceruk.org/prostate-information-and-support/just-diagnosed/other-prostate-problems/enlarged-prostate (Accessed: February 2025)
- Chartier-Kastler E, et al. A prospective, randomized, crossover, multicenter study comparing quality of life using compact versus standard catheters for intermittent self-catheterization. J Urol. 2013;190(3):942-7.
- Hentzen C, et al. What criteria affect a patient’s choice of catheter for self-catheterization? Neurourol Urodyn. 2020;39(1):412-419.


