Community Nurse Specialist Louise Harrison shares a case study highlighting the importance of patient choice when it comes to intermittent self-catheterisation (ISC) and how Curan Lady yielded positive results for a patient who had been experiencing challenges with ISC.
Empowering Patient Choice in Intermittent Self-Catheterisation
The role of intermittent self-catheterisation (ISC) in bladder management
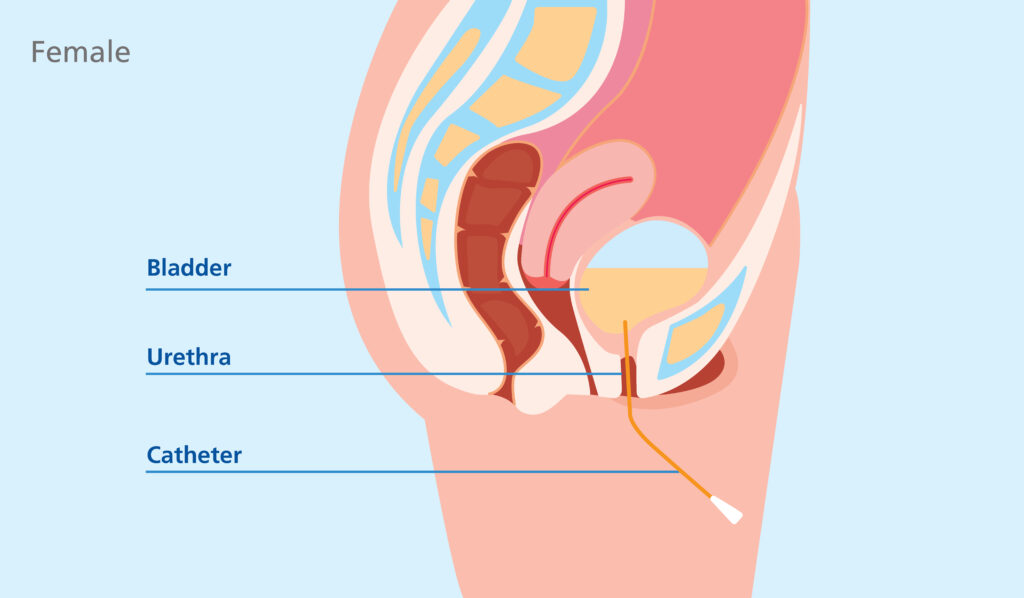
Intermittent self-catheterisation (ISC) is a widely used technique for managing urinary retention and incomplete bladder emptying.1 It involves the periodic insertion of a catheter into the bladder to drain urine, offering an alternative to indwelling catheters and enhancing patient autonomy. ISC is particularly beneficial for individuals with:
- Neurogenic bladder dysfunction, including spinal cord injuries, multiple sclerosis, spina bifida, cauda equina syndrome, or cerebral palsy, which can disrupt normal bladder function2,4
- Bladder outlet obstruction such as benign prostatic hyperplasia (BPH) and urethral strictures, leading to urinary retention2,3
- Detrusor muscle dysfunction, whether due to weak bladder muscles or overactive muscles with impaired emptying, which can lead to incomplete emptying3
- Postoperative urinary retention which may occur temporarily after certain surgeries, affecting the ability to urinate normally1
- Diagnostic or therapeutic procedures such as instilling medications directly into the bladder or onabotulinum toxin A injections.2
By emptying the bladder at regular intervals, ISC can prevent complications such as urinary tract infections (UTIs), incontinence, and kidney damage.1,2 Caution is required, and a thorough assessment will help determine whether the patient is suitable to undertake this method of urine drainage.5
One size may not fit all
For ISC to be successful, the correct catheter choice is crucial – what works well for one patient may not suit another.
Recognising the diverse needs of ISC users, multiple clinical guidelines emphasise the importance of offering patients a choice, ensuring that factors such as dexterity, comfort, and ease of use are considered:
- NICE guidelines recommend that patients be given a choice between single-use hydrophilic or gel-coated catheters, allowing them to select the option that best aligns with their comfort and preferences6
- The Royal College of Nursing (RCN) “Catheter Care” guidance highlights the need for individualised patient assessments to determine whether ISC is suitable and to provide comprehensive education so patients feel confident in performing the procedure independently5
- The European Association of Urology Nurses (EAUN) advises that catheter selection should take into account not only ease of handling and patient comfort, but also how well the catheter fits into a patient’s daily routine and lifestyle.7
Despite these recommendations, many patients struggle with ISC, not because the technique is inherently difficult, but because the catheter they have been provided does not meet their individual needs. Patient needs can evolve over time, and with new or updated catheter options regularly entering the market, it is important to reassess product selection to ensure optimal support for each patient.
This case study illustrates how personalised catheter selection and patient education significantly improved ISC outcomes for a patient facing multiple challenges.
Case overview: ISC challenges in a 41-year-old patient
Sarah is a 41-year-old female patient diagnosed with spina bifida, accompanied by mild learning disabilities and visual impairment. Sarah resides in a residential care facility and uses a wheelchair for mobility.
Sarah had been utilising a standard hydrophilic-coated catheter for ISC but encountered several issues:
- Insertion difficulties: Her limited manual dexterity and poor vision made it challenging to handle and insert the catheter properly
- Urethral trauma: Frequent bleeding during catheterisation suggested possible urethral injury
- Incomplete bladder emptying: Post-void residuals, confirmed with a bladder scanner, indicated that the bladder was not being fully drained
- Recurrent urinary tract infections (UTIs): Incomplete emptying likely contributed to frequent UTIs, impacting her overall health and quality of life.
Intervention: Personalising an ISC solution for Sarah
A comprehensive assessment was conducted by a specialist nurse to better understand how to best help Sarah.
The nurse observed Sarah’s technique to identify any specific difficulties and further discussed proper procedure with Sarah. The nurse also performed a physical examination to assess any anatomical factors that might impede successful catheterisation. Additionally, a post-void bladder scan was performed to evaluate bladder emptying efficiency.
Recognising the need for a more suitable solution, the nurse presented Sarah with a selection of catheter options that could better meet her needs. Among them was the Curan Lady gel catheter, designed to enhance ease of use and comfort. Key features include:
- Hydrogel coating which provides immediate lubrication, reducing friction and discomfort during insertion
- Firmer structure, offering better control, which can be especially beneficial for users with limited dexterity or visual impairments
- User-friendly packaging which accommodates individuals with dexterity challenges.

Outcome: Improved patient experience
When offered the choice, Sarah chose the Curan Lady gel catheter. Switching yielded positive results for Sarah:
- The firmer catheter and hydrogel coating facilitated smoother insertion, minimising trauma and eliminating instances of bleeding
- Sarah found it easier to use than her previous catheter
- The user-friendly design empowered Sarah to perform ISC more comfortably and reliably.
Even after a full year of use, Sarah has continued to choose Curan Lady.
Key takeaways for healthcare professionals
This case demonstrates the power of patient choice, which is critical to improving ISC adherence.
- Providing options allows patients to select catheters that align with their physical abilities and personal preferences
- Assess factors such as manual dexterity, vision, and cognitive function when recommending catheter types
- Comprehensive training and ongoing support are vital to ensure patients feel confident and competent in performing ISC
- Regular follow-ups enable timely identification of issues and adjustments to the catheterisation regimen as needed.
For patients encountering challenges with standard ISC products, exploring alternative options like the Curan Lady gel catheter may offer a viable solution. Assess each patient’s specific needs and preferences to determine the most appropriate catheter choice.
This case study is based on a real patient experience; identifying details have been anonymised to protect patient confidentiality. The information provided is for educational purposes only and should not replace clinical judgment or individualised patient care.
References
- NHS. Intermittent self-catheterisation (ISC) for adults. July 2022. Available at: https://www.gloshospitals.nhs.uk/your-visit/patient-information-leaflets/intermittent-self-catheterisation-isc-adults/ (Accessed: February 2025).
- Prostate Cancer UK. Enlarged prostate: A guide to diagnosis and treatment. May 2022. Available at: https://prostatecanceruk.org/prostate-information-and-support/just-diagnosed/other-prostate-problems/enlarged-prostate (Accessed: February 2025).
- Patient. Intermittent self-catheterisation. April 2023. Available at: https://patient.info/doctor/intermittent-self-catheterisation (Accessed: March 2025).
- National Institute for Health and Care Excellence (NICE). 2023. Urinary incontinence in neurological disease: assessment and management (CG148).
- Royal College of Nursing (RCN). 2021. Catheter Care: RCN guidance for nurses.
- National Institute for Health and Care Excellence (NICE). 2012. Healthcare-associated infections: prevention and control in primary and community care (CG139).
- European Association of Urology Nurses (EAUN). 2024. Urethral intermittent catheterisation in adults: Evidence-based guidelines for best practice in urological health care.


