Pressure Ulcers
A pressure ulcer, also commonly termed ‘bed sore’ or ‘pressure sore’ may be defined as an area of localised damage to the skin and underlying tissue, thought to be caused by a combination of pressure, shear and friction forces. Excessive moisture, sweat and incontinence on the skin surface also lead to excoriation and can render the skin surface vulnerable.
A ‘pressure ulcer’ can be recognised by; persistent erythema, non blanching hyperaemia, blisters, discoloration, localised heat, oedema and indurations and a discoloration in those with darkly pigmented skin1.
Every patient should be assessed to see if they are ‘at risk’ of developing a pressure ulcer, the most recognised scale being the ‘Waterlow’ Score. Patient’s external and internal risk factors should be considered.
Those most ‘at risk’ include patients who are /or have:
- Elderly
- Nutritionally compromised – both the malnourished and the obese
- Immobile / disabled / restricted movement
- Incontinent
- Vascular disease
- Neurological disorder
- Carcinoma
- Medication
Regular skin inspection should continue at each assessment and include close monitoring of the key vulnerable areas; heels, sacrum, tuberosities, trochanters. Patients may be encouraged to inspect their own skin if possible.
Pressure ulcers can be prevented if the patient is assessed correctly and the necessary equipment put in place; pressure therapy equipment (profiling bed, air flow / foam mattresses, cushions) and the correct nursing intervention – turning regimes and regular repositioning.
If a pressure ulcer presents, it should be graded. The most commonly used scale is the EPUAP which grades on a 1 – 4 staging system.
EPUAP2 (European Pressure Ulcer Advisory Panel) grading system
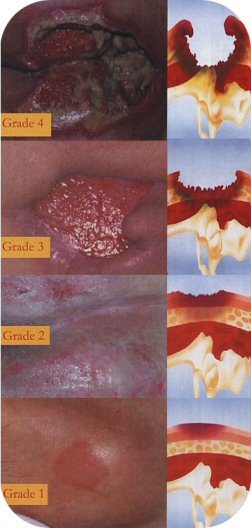 | Grade Four |
Grade Three | |
Grade Two | |
Grade One | |

The principles of best practice with regard to wound management should be adopted in order to resolve symptoms and tissue types at the wound bed and ensure the dressing regime selected maximises patient comfort and supports a moist wound healing interface. Pressure Ulcers are recognised to be chronic wounds which can take time to heal.
Pressure Ulcers are prone to infection and odour and Clinisorb activated charcoal dressing is a useful dressing to use in the management of these symptoms. LBF may also prove valuable in protecting the delicate peri-wound area from exudate and excoriation.
